The name of this condition tells you a lot about it. A "radicle" is any one of the smallest branches of a nerve or blood vessel (from Latin, radicula, the same root for the word "radish") and the "-pathy" suffix indicates an abnormality. Hence, "polyradiculoneuropathy" translates quite literally as "multiple damage of small nerve fibers."
Nobody really knows the exact cause of this disease, but it's associated with raccoon bites, hence the colloquial name. It's believed to be at least triggered by exposure to some as-yet-undefined antigen or antigens in raccoon saliva that mimic normal proteins. The body recognizes something that is normally ignored as "self" as "non-self" and attacks it. The resulting inappropriate immune response causes damage to and demyelination of nerve fibers leading to and controlling skeletal muscle.
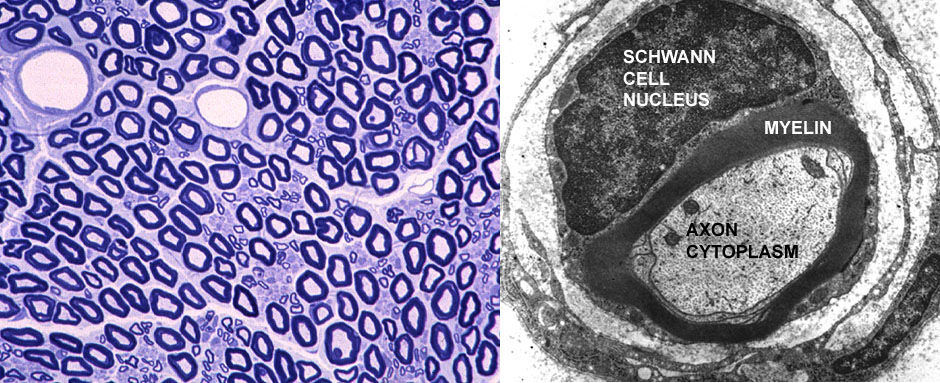
Skeletal muscle must have neural input to contract. Lacking that it begins to atrophy. Furthermore, the progressive nature of the condition means that at first only a few motor units are affected, so the initial symptom is weakness, followed by ataxia (due to inability to control muscles properly) and eventual collapse as more and more motor units in more and more anatomic muscles become affected. In a normal peripheral nerve, seen above in a TB section and as a single axon in the TEM, the myelin sheath is tightly wrapped around the axon. If the plane of section passes through a Schwann cell, its nucleus and cytoplasm are see sitting on top of the transected axon, as at right.
Acute polyradiculoneuropathy is a demyelinating disease: specifically, the auto-immune response to whatever the trigger is strips myelin from the axons. This loss leaves them with sluggish conduction velocities due to charge leakage across the naked plasmalemmal (or no conduction at all), but the axons and the Schwann cells remain intact. This accounts for both the symptoms and the probability of recovery. So Lonesome's muscular weakness is due to a defect in the neural control, not to any inherent damage to the muscle fibers themselves. Given proper supportive care the Schwann cells will re-establish a proper sheath and normal inervation will be restored to the affected myofibers.
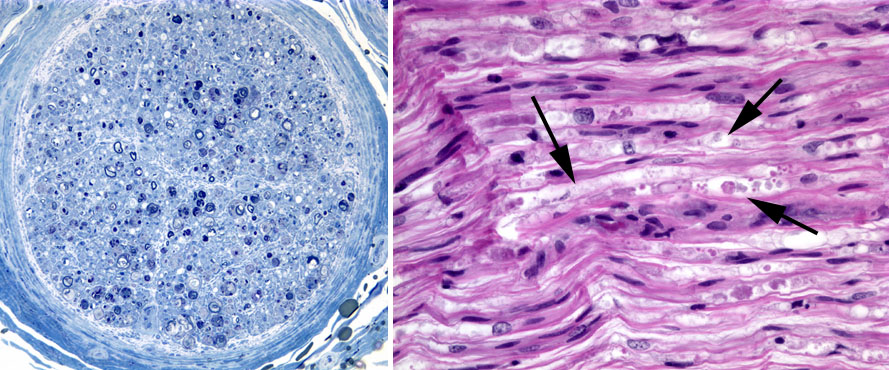
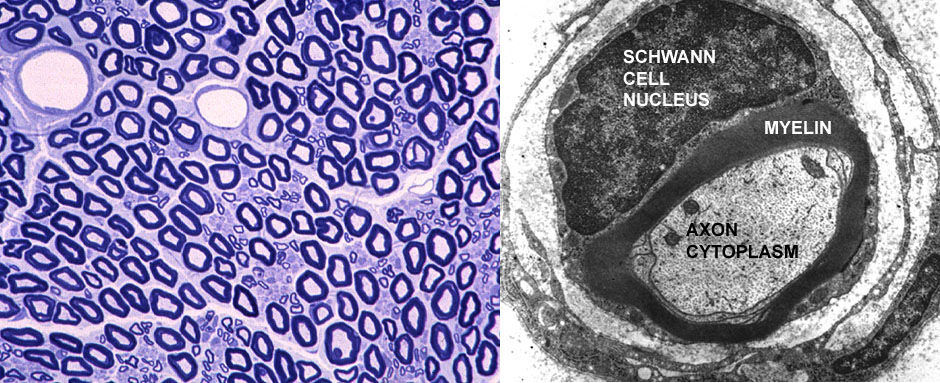
In an affected peripheral nerve, seen at left in a TB stain (cross section) and at right in H&E (longitudinal section) the degeneration of the myelin is pretty clearly visible. The cross section shows few of the stoutly- constructed and strongly-stained sheaths; the longitudinal one shows the loss of normal myelin structure (arrows) and accumulation of lipid residues from its breakdown. The TEM image at left of a normal and a demyelinating axon is pretty graphic: it takes little imagination to recognize that the axon at lower left in this picture not going to be firing properly, any more than an electric wire that's lost its insulation will carry current without a short circuit. Usually, there are no cranial nerve signs; however, in severe cases, the bark may be altered, swallowing impaired, and facial nerve signs be evident. In some cases, respiration is impaired necessitating respiratory support. Had Lonesome's owner been willing to pay for a referral to a specialty clinic that was equipped to do such studies, an EMG (electromyelogram) would have revealed denervation potentials (fibrillation potentials and positive sharp waves) and motor conduction velocity markedly slower than normal in affected nerve fibers, particularly later in the course of the disease.
constructed and strongly-stained sheaths; the longitudinal one shows the loss of normal myelin structure (arrows) and accumulation of lipid residues from its breakdown. The TEM image at left of a normal and a demyelinating axon is pretty graphic: it takes little imagination to recognize that the axon at lower left in this picture not going to be firing properly, any more than an electric wire that's lost its insulation will carry current without a short circuit. Usually, there are no cranial nerve signs; however, in severe cases, the bark may be altered, swallowing impaired, and facial nerve signs be evident. In some cases, respiration is impaired necessitating respiratory support. Had Lonesome's owner been willing to pay for a referral to a specialty clinic that was equipped to do such studies, an EMG (electromyelogram) would have revealed denervation potentials (fibrillation potentials and positive sharp waves) and motor conduction velocity markedly slower than normal in affected nerve fibers, particularly later in the course of the disease.
With all this damage to nerve fibers, the question of why this dog didn't have convulsions needs to be answered, and the answer is simple: all of this takes place in the peripheral nervous system, not in the central nervous system. Demyelination of fibers in the CNS will produce seizures, but the damage here is at the end of the circuit, almost: just before the axons reach the muscles they control. The bodies of the motor neurons are unaffected, and sending out signals, but the signals never reach the effector organs: hence the flaccid paralysis characteristic of the condition. And of course, since the periphery has sensory fibers as well as motor ones, there is an inevitable loss of sensation if those fibers are affected.
 This disorder can affect any age, breed or sex of dog or cat, although the condition is rare before the age of 6 months, probably because the immune system isn't fully developed. A physical exam is usually within normal limits, but the history was a major clue in this case, and an old raccoon bite might be seen in hounds used for hunting, but any dog who tangles with Rocky Raccoon and gets bitten can get it.
This disorder can affect any age, breed or sex of dog or cat, although the condition is rare before the age of 6 months, probably because the immune system isn't fully developed. A physical exam is usually within normal limits, but the history was a major clue in this case, and an old raccoon bite might be seen in hounds used for hunting, but any dog who tangles with Rocky Raccoon and gets bitten can get it.
There is no specific treatment. Corticosteroid therapy may reduce the recovery time, but doesn't reduce the time to reach maximal severity nor the eventual severity. Recent studies support the use of antioxidant steroids (methylprednisolone) to reduce clinical signs. When respiratory depression is evident, this may be helpful. The clinical course is variable and may last from a few days to several weeks. In some cases, there are permanent neurologic deficits, and recovered animals may have recurrences, often more severe than the initial incident. Some cases become chronic.