The tissue of the life to be
We weave with colors all our own,
and in the field of Destiny
We reap as we have sown.
—John Greenleaf Whittier (1807-1892)
Raphael, Stanza 16
SLIDES USED IN THIS EXERCISE: 98-18A, 8, 152, 123, 40, 1-40, 11, 12, 24, LH0180, MCG068, 1210, 723, 54, 28, VM63, VM64, VM65, VM66
THERE ARE PRE-RECORDED LECTURES FOR THIS EXERCISE
Please go to the listing page for these to download and view them
Introduction to Epithelium
Epithelial Classification
Glands and Gland Structure
Salivary Glands
Classically, histologists consider that there are four basic tissues. These are epithelium; connective tissue (which for our purposes includes blood); muscle; and nervous tissue. In this laboratory we will consider the first of these, epithelium.
The term "epithelium" comes from Greek roots: "epi-" = "upon" and "thele" = "breast." Originally this word meant only the skin on the breast, particularly around the nipple, but the term as it's now used covers a good bit wider area than that.
Epithelium may be defined as a relatively avascular and almost wholly cellular (i.e., having little or no connective tissue associated with it) aggregation of cells which are in apposition over a large part of their surfaces, and which are specialized for absorptive, secretory, protective, or sensory activities.
While this definition is useful, you must keep in mind that cells and tissues don't exist independently, and that (with the exception of a smear preparation) you will virtually never see a slide in which only one cell type and/or tissue is present. Epithelia can occur as sheets of cells, as in the lining of the intestine, or as solid aggregations of cells, as in glandular organs. A structural distinction is made between the first type, i.e., "covering and lining epithelium" and the second, which is referred to as "secretory" or "glandular" epithelium.
The neat classification system discussed below is applicable only to "covering and lining" epithelium. Glands and some other organs are "epithelial organs" in that they're made of of cells meeting the basic definition, but obviously, can't be categorized by the same criteria.
"Simple" versus "Stratified" Epithelia: Covering and lining epithelium is classified histologically on the basis of two, and ONLY two, criteria:
1) The number of cell layers present and 2) the shape of the cells in the top layer.
If an epithelial sheet is composed of one and only one layer it is a "simple" epithelium. If there is more than one layer, even if there are only two layers total, then it is a "stratified epithelium."
There is a third category, not so neatly defined, called (for want of a better name) "pseudostratified" epithelium, which will be discussed more fully below.
Cell Shapes
There are three basic cell shapes in covering and lining epithelia: squamous, cuboidal, and columnar. These terms refer to the appearance of cells in microscopic sections. Very often the distinctions between squamous, cuboidal, and columnar shapes are not cut and dried; they may be a matter of opinion and even the aesthetics of the observer.
Simple epithelia can have cells of any shape. Remember that the definitive characteristic of a simple epithelium is that it has only one layer of cells.
Simple Squamous Epithelium
Simple squamous epithelium is easy to find. It forms the lining of the entire cardiovascular system.
The cells of simple squamous epithelium are "fried egg shaped." This can be very difficult to visualize from a section, because in sections the cells are usually cut on edge. But if a sheet of these cells is spread out and viewed en face it becomes much easier to visualize the arrangement. In this drawing, the representation is of a flat sheet of cells butted edge-to-edge. You're seeing them en face, that is, as if you were facing the "wall" of cells. Although it's not shown in this sketch, the cells adhere to each other by forming specialized attachment structures (desmosomes) that give the sheet coherence and strength. Desmosomes are visible only in the electron microscope. There's one nucleus per cell and the limits of each cell are well defined. Even though the nucleus isn't seen in every cell, each one does have a nucleus; sometimes it's on the opposite side of the plane and can't be visualized.
Blood vessels are lined with simple squamous epithelium—in fact, the entire cardiovascular system is. In the image above, a vein is running through the substance of the pancreas. The lumen is filled with red-stained erythrocytes. The nuclei of the mural epithelial cells are visible as purplish cigar-shaped objects running parallel to the long axis of the vein. Because squamous cells have very little cytoplasm, and because here you're viewing them on edge, the nuclei are about all that's visible.
Simple squamous epithelium isn't well suited to places where there's wear and tear. It's quite fragile, and the places where the edges of cells are butted up against one another are weak points. It's usually found in places like this, where its "slick" surface facilitates flow of fluids.
Slide 8 contains an artery, a vein, and a nerve, all cut in cross section. The artery has the thickest wall of the three; the nerve has numerous smaller profiles inside it. Examine the innermost wall of the artery at high magnification; you'll be able to see that it's completely covered with simple epithelium. You are viewing these cells (as is almost always the case with this type of epithelium) along their cut edge, so the cytoplasm is virtually invisible because the cell is so thin. About all that can be clearly seen is the nuclei bulging into the lumen. In virtually any tissue section, you will be able to find a blood vessel, and all of them have this same type of lining. Usually the muscular wall of the artery contracts from the fixative, and the nuclei bulge into the lumen, making them a little easier to spot.
Here's another example of simple squamous epithelium. The organs of the body are covered with peritoneum, a smooth and glistening connective tissue investment that allows them to slide past one another. The peritoneum is double-layered, with a sheet of squamous cells on each side, and between them a bit of connective tissue carrying blood vessels (as we'll see in Exercise 5, only connective tissue can form blood vessels). The smooth and somewhat secretory simple squamous cells are adjacent to the organs, and there are two layers, back to back. It's pretty easy to distinguish the differences between the nuclei of the squamous epithelial cells and those of the epithelial cells forming the walls of the capillaries. This slide is stained with Masson's method and the greenish wisps of material are the fibers of the connective tissue between the two layers.
Since the peritoneal lining of the is derived from the embryonic mesoderm, this specific example is sometimes called "mesothelium." Epithelial cells and epithelial organs may be formed by any of the three primary germ layers (ectoderm, mesoderm, and endoderm) and it's important not to confuse the term "epithelium" with "epiderm." In this respect the term "mesothelium" is unfortunate, but it's firmly fixed in the literature and you should be familiar with it. Epithelium is epithelium, regardless of what embryonic layer it's derived from.
Simple Cuboidal and Simple Columnar Epithelium
Simple cuboidal epithelium is classically demonstrated in the ductwork of exocrine glands. It's found in many other sites, too. To be "cuboidal" the cells should be about as high as they are wide, but sometimes whether a given epithelial sheet is cuboidal or columnar is a matter of judgment and even artistic sense!
 Simple cuboidal epithelium, by definition has only ONE layer of cells, which is separated from an underlying connective tissue support by a basement membrane (BM). The basement membrane is a fairly complicated structure but in a light micrograph about all you will see is a denser line of color, which is a good deal easier to make out if you use a special stain like the periodic acid/Schiff method for carbohydrates. This sketch shows the layout of simple cuboidal epithelium and the underlying BM. The cells are approximately as tall as they are wide. Remember: you're seeing two dimensions, but these cells have depth, too, and they aren't really "cubes" in three dimensions. The shape, viewed from the top, is more or less hexagonal. But in a section all you see is the edges, and they appear as if they were cube-shaped.
Simple cuboidal epithelium, by definition has only ONE layer of cells, which is separated from an underlying connective tissue support by a basement membrane (BM). The basement membrane is a fairly complicated structure but in a light micrograph about all you will see is a denser line of color, which is a good deal easier to make out if you use a special stain like the periodic acid/Schiff method for carbohydrates. This sketch shows the layout of simple cuboidal epithelium and the underlying BM. The cells are approximately as tall as they are wide. Remember: you're seeing two dimensions, but these cells have depth, too, and they aren't really "cubes" in three dimensions. The shape, viewed from the top, is more or less hexagonal. But in a section all you see is the edges, and they appear as if they were cube-shaped.
This section of pancreas from slide 34 shows a small duct in the center of the field. The wall of the duct is made of simple cuboidal epithelium. Exocrine gland ducts of this type are made of cuboidal cells arranged like bricks in a wall. As he duct enlarges there may be a transition from cuboidal to a columnar shape. As was mentioned above, the distinction between "high cuboidal" and "low columnar" is sometimes a matter of opinion and aesthetics. In ducts there's a gradation from an indisputably "cuboidal" duct wall (such as this one) to the obviously columnar walls of much larger ducts. Furthermore, as ducts really increase in size the epithelium can stratify. As with columnar epithelium, you wouldn't expect to find the cuboidal type in regions where abrasion is likely. The "covering and lining" nomenclature used to describe the duct isn't applicable to the secretory regions. There are a number of these visible in the image. They fall into the subdivision of "glandular epithelium" as they are solid masses of tissue.
Simple columnar epithelium is very common: it comprises most of the lining of the digestive tract and the walls of medium sized gland ducts. You'll easily see it on slide 123 in the lumen of the gall bladder, and on slide 40, where tall absorptive cells make up the bulk of the lining of the duodenum.

Compare the sketch above to the actual specimen of gall bladder epithelium to the right. There is one and only one layer of cells, and in the section you can even make out the location of the basement membrane underlying these cells. Simple columnar epithelium is found in places where there is minimal wear-and-tear, and which aren't subject to abrasion. It's a rather fragile type, typically specialized for absorption or secretion. It usually has structural specializations to carry out these functions: the brush border of microvilli is the best example.
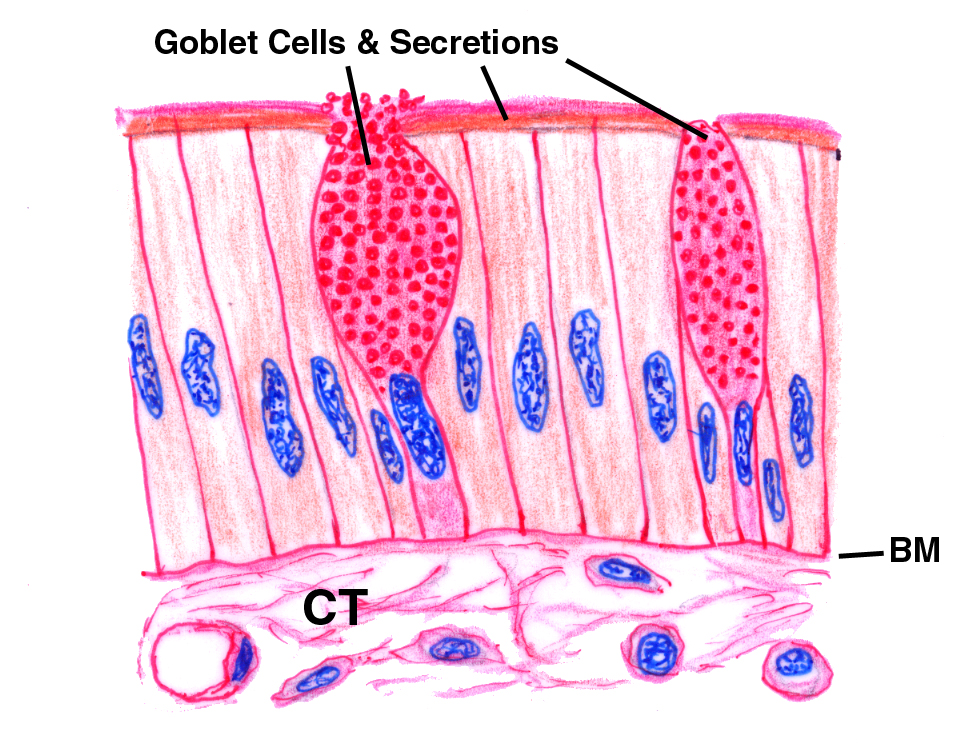 Goblet Cells
Goblet Cells
 A feature of the lining epithelium of the intestine as seen in slide 40 is the presence of goblet cells. The epithelial sheet isn't entirely
uniform: there's more than one cell type present. Epithelial sheets
of this type usually (not always) contain goblet cells, which
appear as large clear spaces here and there among the columnar absorptive
cells. The name comes from the cup-like shape of these cells. The
"cup" is filled with mucus droplets that are released into the lumen
of the tract. Goblet cells are actually unicellular exocrine glands. They're found in a couple of places in addition to the intestine. Their secretions are used to produce a protective film over the surface of the absorptive cells of the small intestine; and a lubricant in the large intestine to help move the fecal bolus on its way. They're also found in the epithelium lining the inside surface of the eyelids, and in the air passages of the respiratory system. Goblet cell secretions are mostly mucous in composition, so it's no surprise that they're PAS-positive.
A feature of the lining epithelium of the intestine as seen in slide 40 is the presence of goblet cells. The epithelial sheet isn't entirely
uniform: there's more than one cell type present. Epithelial sheets
of this type usually (not always) contain goblet cells, which
appear as large clear spaces here and there among the columnar absorptive
cells. The name comes from the cup-like shape of these cells. The
"cup" is filled with mucus droplets that are released into the lumen
of the tract. Goblet cells are actually unicellular exocrine glands. They're found in a couple of places in addition to the intestine. Their secretions are used to produce a protective film over the surface of the absorptive cells of the small intestine; and a lubricant in the large intestine to help move the fecal bolus on its way. They're also found in the epithelium lining the inside surface of the eyelids, and in the air passages of the respiratory system. Goblet cell secretions are mostly mucous in composition, so it's no surprise that they're PAS-positive.
Stratified epithelia are those composed of more than one layer of cells. It is important to remember that a stratified epithelium is classified on the basis of the shape of the cells in the TOP LAYER ONLY. Cells in the lower layers may take any shape, and often do.
Stratified Squamous Epithelium
Stratified squamous epithelium is the most common stratified type. It lines the oral cavity, the anus, the vagina, and several other openings. The lumen of the esophagus is lined with it, too. The external skin is an extensive sheet of stratified squamous epithelium, with specialization for resistance to abrasion.
The example above is from the vagina. Notice that there are 10-20 layers of cells present, which by definition makes this a "stratified" epithelium; and that the cells at the free surface are flattened, squamous shaped ones, hence "stratified squamous" is the correct characterization of this form. Note also that the cells in the deeper layers can be any shape (though most of them could be described as cuboidal). That's irrelevant to the characterization of the epithelium; what counts is the shape of cells at the top.
The best example of stratified squamous epithelium is the skin: the general body surface is covered with it, as slides 7 and 11 demonstrate. Slide 7 (left, above) is made from thin skin; slide 11 is made from thicker skin. Both of them, however, are classified as "stratified squamous." Both also illustrate the keratinization of stratified squamous epithelium.
Keratinization is the process of making the top layer(s) of a stratified squamous sheet hardened and dead. It's an adaptation to wear and tear found on abraded surfaces. Not all stratified squamous epithelial sheets are keratinized, but most are. Very heavy keratinization can be seen on slide 24 (above, at right). This example is from the footpad of a dog.
Keratinization is an inherent metabolic activity of the places where it's found. That is, usually no external forces are needed to induce it to occur, though such forces can accelerate it. Think about the footpads on a newborn puppy: they're quite soft and velvety, but as the pup ages and uses his feet, the pads get hardened and rough. If you looked at those footpads on the day of birth, however, you'd see that there was in fact some keratinization present. It increases as the dog ages, but he's born with it.
One other point needs to be made about this process. Some texts will tell you that "wet" stratified squamous epithelium doesn't keratinize, but "dry" stratified squamous does. THIS IS NOT CORRECT. Keratinization can and does occur on "wet" surfaces: the lining of the oral cavity and the esophagus in domestic animals is usually keratinized (whereas in humans it isn't). Keratinization normally occurs only in stratified squamous epithelium, not in other stratified types. If it's found in places where it's not supposed to be, it's an indication of something seriously wrong.
Cuboidal and columnar epithelia can stratify: this is fairly common in large ducts of exocrine organs. Stratified cuboidal epithelium is more commonly seen than stratified columnar, but both categories exist. The example below (right) is from slide 1210: it's the duct of one of the salivary glands embedded in the tongue. The epithelium of the duct is distinctly stratified into two layers, and the top layer is cuboidal. Hence, using the nomenclature convention for "covering and lining" epithelia, this is a true stratified cuboidal type. Notice that the stratification isn't uniform from one place to another. As the duct enlarges, though, it becomes more likely that a section will show very clearly stratified epithelium. In some of the very largest ducts, such as the mammary gland, it will grade into stratified columnar. Try slide 28 and examine the larger ducts to find this type of epithelium.
Pseudostratified Epithelium
In this imperfect world, nothing is as simple as we'd like it to be, and it's time to consider pseudostratified epithelium. This is usually treated as a separate category, although in fact it is a subset of the simple form. In pseudostratified epithelium, the general appearance is that of several layers, but in reality all of the cells reach the basement membrane, and the epithelium is truly a simple one. Since all of the cells do rest on the basement membrane there is only one layer, although the location of nuclei at different levels gives the specious appearance that more than one exists. This is easy to demonstrate in an electron micrograph, or with some special stains, but very hard to verify with only H&E staining.
The best examples of pseudostratified epithelium are found in the respiratory system. Slides 26 (trachea) and 115 (which includes part of the nasal cavity) provide examples of this type of epithelium. Most of the upper respiratory tree is lined with pseudostratified columnar epithelium. This image is from slide 115. Note that in this case there are goblet cells present in the epithelial sheet, and that the non-goblet cells are ciliated:
Pseudostratified epithelium is usually ciliated; but sometimes it isn't. And goblet cells don't have to be present, either, though they are in most pseudostratified epithelia. There are several examples of unciliated pseudostratified epithelium in mammals.
Notice that the cells in the deep layers are cuboidal to columnar; that those of the topmost layer are larger, pale and washed out looking, with small nuclei; and that the border is "scalloped." These are the definitive characteristics of this epithelial type. There may be pink colored so-called "inclusion bodies." That term, which is widely used in the literature, is a misnomer. These aren't true inclusions: instead they're areas of extra plasma membrane that has been folded up into a relatively small space and internalized. Why do this? The urinary bladder (as is obvious to all of us) has to expand and contract as the amount of stored urine increases or decreases. The epithelium you see here is in a bladder that's contracted (because it's empty...ahhh....).To accommodate this change in organ volume, the lining epithelium has to have extra membrane so that when the bladder is distended, the cells aren't stretched and torn. The extra membrane has to go somewhere, and where it goes is into these neatly folded "lenticular bodies" that are, in fact, continuous with the surface of the cell. You can envision this in the same way you might see lettering on a half-deflated balloon, with wrinkles in its sides.
Urinary epithelium is impermeable to water, thanks to large numbers of occluding junctions between the cells. This impermeability protects the urinary tract from damage caused by the presence of hypertonic urine, and also prevents dilution of the urine by osmosis. Only mammals and birds can produce urine that's hypertonic to their body fluids (We'll discuss this process in the exercise on the urinary system elsewhere on this CD) and having these sealed spots is important, because loss of fluid from the intercellular compartment would be a serious matter.
Glands are "epithelial organs." These are treated separately for purposes of classification; the "covering and lining" categories don't apply to masses of cells. A discussion of the structural classification of glands is provided elsewhere.
One of the features of epithelia which has a great deal of clinical significance
is its capacity for regeneration. In most epithelia, production of new cells is
a more or less constant process, and one can express the activity of a tissue
in terms of it mitotic index, the ratio of dividing cells to
non-dividing ones. A good example of the mitotic activity of epithelia is shown at the right. This is from slide 40, a section from the small intestine. Deep down in the layers of the epithelium,
right near where the luminal covering meets the underlying connective tissue,
you'll frequently find mitotic figures. These are evidence of cellular
proliferation and appear as dense irregular shapes where the nuclei would
normally be located. All of the different stages are represented—prophase,
anaphase, metaphase, and telophase—but there's no point in trying to pick
them out. Much more clearly defined mitotic figures can be seen on slide 54, a
developing whitefish embryo.
It's worth adding that while mitotic figures are common in most epithelia, they aren't in all epithelia, and when they aren't supposed to be there, something is wrong. For example, you certainly wouldn't expect a high mitotic index in a normal salivary gland or in the kidney, though these are both epithelial organs. A high MI in the intestine is an adaptation to rapid loss of cells; in other places it's a sign of uncontrolled cell division and one of the hallmarks of cancer.
There's clinical adaptation of this concept. Nuclear medicine and radiation therapy is based on the understanding that that a tissue is sensitive to radiation exposure in direct proportion to its rapidity of division. This is the "Law of Bergonié," (named for Jean A. Bergonié (1857-1925) a French physician). It follows from this rule that exposure of rapidly proliferating, epithelia to radiation will have marked effects, both therapeutic and deleterious. Irradiation of a tumor kills tumor cells first, but it also affects epithelia that are supposed to divide rapidly. Overdose an animal with x-rays, and symptoms include diarrhea, vomiting, and loss of hair. The rapidly dividing cells of the gastrointestinal tract and the hair follicles, just like tumor cells, are sensitive and get killed.
The cross section of mouse intestine shown on the right provides a nice example of just how proliferative an epithelial sheet can be. At first glance you might take this to be a PAS stain; but it isn't. It's been subjected to immunolabeling to show the location of RNA and to identify cells producing it in quantity—that is, cells actively dividing.
First the animal was treated with bromo-deoxyuridine (BRDU). BRDU is a uridine derivative that stops RNA synthesis by replacing normal uridine in the forming RNA strand. RNA is made in the nucleus, so the BRDU is bound there. On tissue sections the sites where BRDU was present were labeled with an anti-BRDU antibody, and the complex of BRDU and antibody was then rendered visible with a colored "tag." The section was counterstained with H&E to provide structural information.
In this image, the rapidly-dividing cells of the intestinal mucosa are clearly demonstrated. Their nuclei have taken up large amounts of BRDU, and hence are strongly labeled. Most of the label is in the deep region of the epithelium*. In every one of these locations you might find a mitotic figure in a routine stain. Mucosal epithelium is very proliferative; the life of an average cell is 7-10 days. This rapid turnover is needed to deal with the harsh environment in which these cells must live. You would get similar results in almost any epithelial sheet.
*Compare this image to the example given in Exercise 2 of PAS staining, and you'll see that in that case, the goblet cells are scattered throughout the epithelial sheet, not concentrated in one area as they are here. My sincere thanks to Dr. Kevin McDorman, VMRCVM Class of 1995, for this image.